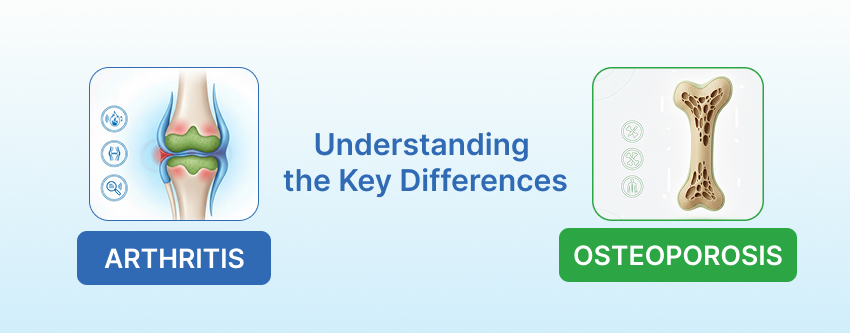
Healthy bones and joints are essential for staying active, independent, and enjoying everyday life. Two common conditions that affect this system are arthritis and osteoporosis, and they impact the body in very different ways. Arthritis mainly leads to joint pain and inflammation, while osteoporosis gradually weakens the bones leading to fractures, often without any noticeable symptoms in the early stages.
Millions of people around the world live with these conditions, and in India, many adults experience joint discomfort or reduced bone strength without realising it. This makes awareness, early detection, and proper care crucial for maintaining mobility and overall well-being.
Recognising the differences between arthritis vs osteoporosis can help you spot symptoms early, take preventive measures, and seek expert care. At Venkateshwar Hospital, a NABH-accredited multi-speciality hospital in Dwarka, patients benefit from advanced diagnostics, specialised treatment plans, and personalised guidance from experienced orthopaedic and rheumatologists.
What is Arthritis?
Arthritis is a medical condition that affects the joints, causing pain, stiffness, and inflammation. It is not a single disease but a term used for more than 100 different joint disorders that can affect people of all ages.
Focus of the Condition
The condition primarily targets the joints, leading to discomfort, swelling, and a reduced range of motion. Over time, arthritis can make everyday activities like walking, climbing stairs, or holding objects difficult lead to joint deformity.
Types of Arthritis
- Osteoarthritis (OA): The most common form, caused by the gradual wear and tear of the cartilage that cushions the joints. It often affects the knees, hips, hands, and spine.
- Rheumatoid Arthritis (RA): An autoimmune condition where the body’s immune system mistakenly attacks the joints, causing inflammation and joint damage. RA commonly affects the hands, wrists, and feet.
- Other Types: Includes psoriatic arthritis, gout, and connective tissue disease , which may have different causes and symptoms.
Common Symptoms
- Persistent joint pain and stiffness
- Swelling, warmth, or redness around affected joints
- Limited flexibility or range of motion
- Joint deformities in advanced stages
Common Causes
- Age-related wear and tear on joints
- Previous joint injury or trauma
- Autoimmune disorders (e.g., rheumatoid arthritis)
- Overuse of joints due to repetitive activities or sports
- Genetic factors
Also Read – Why are women prone to joint issues?
What is Osteoporosis?
Osteoporosis is a bone disease in which the density and quality of bone are reduced, making the bones fragile and more likely to break. It is sometimes called a “silent disease” because it often progresses without noticeable symptoms until a fracture occurs.
Focus of the Condition
The condition primarily affects the bones, leading to reduced strength and increased risk of fractures, even from minor falls or injuries. Commonly affected areas include the spine, hips, and wrists.
Common Symptoms
- Often, there are no symptoms in the early stages.
- Back pain caused by a collapsed or fractured vertebra
- Loss of height over time
- Stooped posture, sometimes referred to as kyphosis.
- Fractures of the hip, spine, or wrist from minimal trauma
Common Causes
- Ageing, which naturally reduces bone density
- Hormonal changes, especially in postmenopausal women, are due to reduced oestrogen levels
- Inadequate intake of calcium and vitamin D
- Sedentary lifestyle or lack of weight-bearing exercise
- Long-term use of certain medications, such as corticosteroids
- Genetic factors and family history of osteoporosis
Arthritis vs Osteoporosis: Key Differences
Understanding the differences between arthritis vs osteoporosis is important because, although both affect the musculoskeletal system, they target different structures and require different approaches to management. Recognising these key differences can help in early detection, preventive measures, and seeking appropriate medical care.
| Feature | Arthritis | Osteoporosis |
| Primary Focus | Affects the joints, causing inflammation, pain, and reduced mobility | Affects the bones, leading to reduced density, fragility, and higher fracture risk |
| Cause | Inflammation, autoimmune conditions (like rheumatoid arthritis), or wear and tear of cartilage (osteoarthritis) | Bone thinning due to ageing, hormonal changes (especially post-menopause), nutritional deficiencies, sedentary lifestyle, or long-term medication use |
| Symptoms | Joint pain, stiffness, swelling, warmth, and reduced range of motion | Often silent until a fracture occurs; back pain, height loss, stooped posture, hip/spine/wrist fractures |
| Visibility | Swelling, redness, or warmth around affected joints may be visible | Usually undetected until a fracture or bone loss is confirmed via medical tests |
| Impact Area | Specific joints such as knees, hips, hands, or spine | The entire skeletal system, particularly the spine, hips, and wrists |
Also Read – Top Signs You Need the Best Orthopedic Doctor in Dwarka
Can You Have Both?
It is possible for an individual to have both arthritis and osteoporosis, particularly in older adults. While these conditions affect different parts of the musculoskeletal system, arthritis impacts the joints and osteoporosis affects bone density. They can coexist and sometimes influence each other. For instance, reduced mobility from arthritis may contribute to bone weakening, increasing the risk of osteoporosis.
When considering arthritis vs osteoporosis, it is important to recognise that each condition has distinct causes, symptoms, and treatment approaches. Arthritis management focuses on reducing joint inflammation and pain, maintaining flexibility, and improving mobility, while osteoporosis care prioritises strengthening bones, preventing fractures, and ensuring adequate nutrition and lifestyle support.
Because these conditions differ, an accurate diagnosis by a healthcare professional is essential. Understanding the nuances of arthritis vs osteoporosis allows for personalised interventions that protect both joint and bone health, helping to maintain overall quality of life and reduce potential complications.
Diagnosis and Medical Tests
Accurate diagnosis is essential when distinguishing arthritis vs osteoporosis, as the two conditions affect different parts of the musculoskeletal system and require different management approaches.
Arthritis Diagnosis
Arthritis is primarily diagnosed through a combination of clinical evaluation and imaging tests:
- Physical examination: Doctors assess joint swelling, tenderness, warmth, range of motion, and deformities.
- X-rays: Help detect joint damage, cartilage loss, and bone changes.
- MRI (Magnetic Resonance Imaging): Provides detailed images of cartilage, ligaments, and soft tissues to detect early or subtle joint damage.
- Blood tests: Useful for identifying autoimmune forms like rheumatoid arthritis, by checking for specific antibodies and markers of inflammation.
Osteoporosis Diagnosis
Osteoporosis is diagnosed by assessing bone density and fracture risk:
- DEXA (Dual-Energy X-ray Absorptiometry) scan: The standard test for measuring bone mineral density, typically at the hip and spine.
- Medical history and risk assessment: Evaluates factors such as age, hormonal status, previous fractures, family history, medications, lifestyle, and nutrition.
Role of Medical History and Physical Exams
For both conditions, a thorough medical history and physical examination are crucial. They help the healthcare professional understand symptoms, identify risk factors, and guide appropriate diagnostic tests. Accurate evaluation ensures that interventions for arthritis vs osteoporosis are targeted effectively, protecting joint function and bone health while reducing the risk of complications.
Treatment Options
Managing arthritis and osteoporosis requires approaches suited to each condition.
Arthritis
- Medications: Pain relievers and anti-inflammatories can ease discomfort.
- Physical therapy: Gentle exercises help maintain joint flexibility and strength.
- Joint injections: Corticosteroids or hyaluronic acid may reduce inflammation.
- Lifestyle changes: Maintaining a healthy weight and doing low-impact activities like swimming or cycling keeps joints mobile.
Osteoporosis
- Supplements: Calcium and Vitamin D support stronger bones.
- Medications: Bone-strengthening drugs such as bisphosphonates help reduce fracture risk.
- Exercise: Weight-bearing and resistance exercises strengthen bones.
- Fall prevention: Simple home adjustments and balance exercises can lower the chance of fractures.
Preventive Measures
Maintaining strong bones and healthy joints is key to reducing the risk of arthritis and osteoporosis as we age. Simple lifestyle habits can make a significant difference:
- Balanced diet: Include calcium-rich foods such as dairy, leafy greens, and fortified products, along with Vitamin D to support bone strength.
- Regular physical activity: Engage in exercises that are gentle on the joints but strengthen muscles and bones, such as walking, swimming, yoga, or light resistance training.
- Avoid smoking and limit alcohol: Smoking and excessive alcohol can weaken bones and worsen joint health over time.
- Regular screenings: Periodic bone and joint check-ups, especially after the age of 50, help detect early changes and allow timely interventions.
Adopting these preventive measures supports long-term mobility, reduces fracture risk, and helps maintain overall musculoskeletal health.
Conclusion
When considering arthritis vs osteoporosis, it is important to understand that these conditions affect the body differently. Arthritis mainly impacts the joints, leading to pain, stiffness, and inflammation, while osteoporosis primarily weakens bones, increasing the risk of fractures, often without early warning signs.
Recognising these differences allows for timely diagnosis and personalised care. By monitoring symptoms, maintaining a healthy lifestyle, and consulting a healthcare professional, you can protect both joint and bone health, preserve mobility, and improve overall quality of life.
If you experience persistent joint pain, stiffness, or signs of bone fragility, seek medical advice promptly for proper evaluation and treatment.
Also Read – Knee Pain Causes: When to Consider Seeing an Orthopaedic Surgeon
Frequently Asked Questions
1. Can arthritis lead to osteoporosis?
Arthritis itself does not directly cause osteoporosis. However, reduced mobility due to joint pain chronic inflammation or long-term use of certain medications like corticosteroids may increase the risk of bone weakening over time.
2. At what age do arthritis and osteoporosis usually begin?
Osteoarthritis is most common after age 50. Rheumatoid arthritis can occur earlier, sometimes in young adults. Osteoporosis usually develops after 50, particularly in women after menopause, because of hormonal changes.
3. Is joint pain a symptom of osteoporosis?
No. Osteoporosis typically does not cause joint pain. Its main effect is weakened bones, which increases the likelihood of fractures. Persistent joint pain is more often related to arthritis.
4. Are osteoarthritis and osteoporosis the same?
No. Osteoarthritis affects the joints due to cartilage wear and tear, while osteoporosis is a bone condition that reduces bone density and strength. Understanding arthritis vs osteoporosis helps distinguish the two.
5. Which condition causes more fractures?
Osteoporosis increases the risk of fractures, especially in the hip, spine, and wrist. Arthritis does not directly cause fractures, but it may raise the risk of falls because of joint stiffness or pain.
6. Is exercise safe if I have either condition?
Generally, low-impact exercises such as walking, swimming, and strength training support joint flexibility in arthritis and help maintain bone strength in osteoporosis. Professional guidance can help tailor safe activity levels.
7. How is rheumatoid arthritis different from osteoporosis?
Rheumatoid arthritis is an autoimmune condition where the immune system attacks the joints, causing inflammation and damage. Osteoporosis involves reduced bone density and fragility, usually from age, hormones, or lifestyle factors, and is not autoimmune.
8. What are the risk factors for both conditions?
Common risk factors include ageing, family history, insufficient physical activity, poor nutrition, smoking, and excessive alcohol intake. Women, especially after menopause, are at higher risk for both arthritis and osteoporosis.
Medically Reviewed by — Dr. Sakshi Mittal (Sr. Consultant – Rheumatology)